
Active Ingredients
on
Skin care
peer-reviewed
Amazonian Oils Blend calms sensitive skin while rebalancing skin microbiota
MARIA CELIA REIMBERG1; SANDRINE DELAUNOIS*2; CÉCILE DELLUC2; HANANE CHAJRA2, MATHILDE FRECHET2
*Corresponding author
1 Beraca Ingredientes Naturais, São Paulo, Brazil
2 Lucas Meyer Cosmetics by Clariant, Toulouse, France
ABSTRACT: Sensitive skin, a globally prevalent condition impacting millions of people, disrupts skin equilibrium, resulting in sensations such as itching, redness, and discomfort. Marketed products, including those containing CBD, a phytocannabinoid molecule endorsed in Cannabis sativa oil, promise soothing effects, but regulatory challenges exist for this molecule. An alternative, an ethically sourced Amazon oil blend rich in beta-caryophyllene, alpha-humulene, and linoleic acid, exhibits cannabimimetic properties. In inflammatory contexts, the blend surpasses CBD in soothing effects by enhancing beta-endorphin secretion. Clinical effects demonstrate a visible improvement in skin condition after 28 days by reducing redness, itching, and IL-6 levels. Furthermore, the blend promotes the recovery of normal skin microbiota, enhancing the microbiome's preservation for healthier skin.
??????????????????
“
“A study in healthy women providing probiotic yogurt for four weeks showed an improvement in emotional responses as measured by brain scans”
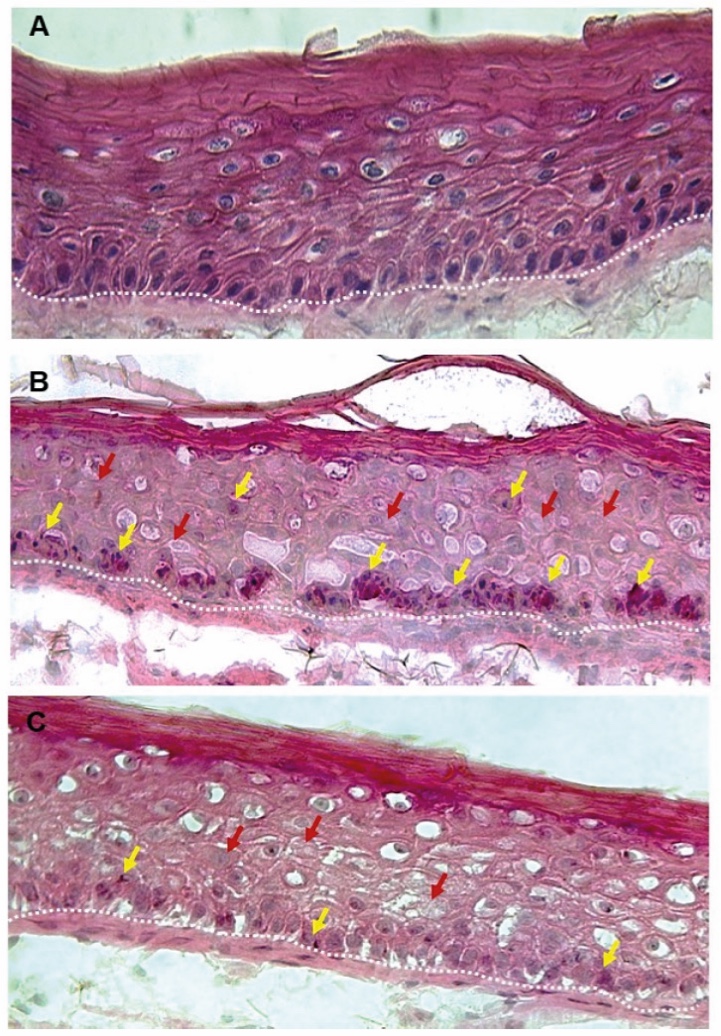
Figure 1. Skin Section with Microbiome. Most microorganisms live in the superficial layers of the stratum corneum and in the upper parts of the hair follicles. Some reside in the deeper areas of the hair follicles and are beyond the reach of ordinary disinfection procedures. There bacteria are a reservoir for recolonization after the surface bacteria are removed.
Materials and methods
Studies of major depressive disorder have been correlated with reduced Lactobacillus and Bifidobacteria and symptom severity has been correlated to changes in Firmicutes, Actinobacteria, and Bacteriodes. Gut microbiota that contain more butyrate producers have been correlated with improved quality of life (1).
A study in healthy women providing probiotic yogurt for four weeks showed an improvement in emotional responses as measured by brain scans (2). A subsequent study by Mohammadi et al. (3) investigated the impacts of probiotic yogurt and probiotic capsules over 6 weeks and found a significant improvement in depression-anxiety-stress scores in subjects taking the specific strains of probiotics contained in the yogurt or capsules. Other studies with probiotics have indicated improvements in depression scores, anxiety, postpartum depression and mood rating in an elderly population (4-7).
Other studies have indicated a benefit of probiotic supplementation in alleviating symptoms of stress. In particular, researchers have looked at stress in students as they prepared for exams, while also evaluating other health indicators such as flu and cold symptoms (1). In healthy people, there is an indication that probiotic supplementation may help to maintain memory function under conditions of acute stress.
INTRODUCTION
The escalating global incidence of sensitivity-related skin conditions within both the general population and those afflicted by facial dermatitis underscores growing concern. Beyond the subjective discomfort associated with sensitive skin, an imbalanced microbiota further complicates the condition.
Characterized by distressing sensations, including stinging, burning, pain, pruritus, and tingling, sensitive skin manifests in response to stimuli that under normal circumstances should not provoke such heightened sensibility. These discomforting experiences lack an explanatory basis in skin lesions attributable to any identifiable skin disease, with the skin often appearing normal or displaying sustained erythema. Common triggers for skin reactions include chemical factors, notably cosmetics and poor water quality, and environmental factors, especially solar exposure and UV radiation.
The extensive prevalence of sensitive skin within the population, as highlighted by various epidemiological studies, has piqued significant interest in the cosmetic industry. A substantial number of individuals, both men and women, self-identify as having sensitive skin, creating a substantial demand for products designed to alleviate skin sensitivity [1].
The sensitivity of the skin is provoked by stimuli acting on skin cells, initiating an inflammatory cascade that culminates in the release of various inflammatory cytokines, including IL-1β, IL-6, and IFN-γ. In this study, we specifically quantify IL-6 due to its pivotal role in acute and chronic skin inflammation. IL-6 plays a crucial role in the initial stages of inflammation, promoting increased expression of epidermal proliferation and dermal fibroblasts [2], leading to side effects such as edema and redness. Notably, IL-6 is produced in response to immediate and transient environmental stress factors [3].
Given these specificities, we have chosen to evaluate the effect of Amazon Oils Blend on IL-6 production, considering its potential to soothe sensitive skin in a cosmetic formulation focused on well-being. Additionally, we investigate the impact of the product on the microbiota of sensitive skin, recognizing the interconnectedness of skin conditions, microbiota, sensitivity, and barrier function. Although consensus is lacking regarding the bacterial genera involved in skin sensitivity, maintaining a well-balanced microbiota is crucial for the development of new skincare products [4].
Previous studies have shown no significant correlation in microbiome diversity (Shannon index) between healthy and sensitive skin [5,6,7]. Our research focuses on specific bacterial genera, such as Micrococcus, Corynebacterium, and Kocuria, which are notably expressed in sensitive skin according to cosmetic field studies [8,9,10].
In light of our findings, the association with cannabidiol (CBD) emerges as a promising solution for alleviating sensitive skin symptoms. This phytocannabinoid, primarily identified in hemp seed oil, is renowned for its medicinal properties, including anti-seizure, anti-inflammatory, and mood-regulating effects. In the realm of cosmetics, CBD is increasingly incorporated into formulations for protection, hydration, care, and addressing sensitivity.
CBD exerts its effects by binding to CB1 or CB2 receptors within the endocannabinoid system, facilitating pain modulation, anti-inflammatory responses, and overall well-being. Notably, CB2 receptors, influencing various body parts including the skin, trigger the release of beta-endorphin, associated with a sensation of skin well-being and relief in sensitive skin.
To this end, we have developed a cannabimimetic blend of Amazon oils rich in beta-caryophyllene, a natural phytocannabinoid. As an alternative to CBD, this blend aims to rebalance the skin microbiota, presenting considerable interest for both cosmetic and dermatological applications. Beta-caryophyllene, a major compound in this oil blend, modulates the endocannabinoid system by activating cannabinoid receptor-type 2 (CB2), influencing the release of cytokines and neurotransmitters, particularly beta-endorphin, linked to skin well-being. This ethically sourced Amazonian Oil Blend adheres to sustainable practices, aligning with a program that ensures compliance with Biodiversity Laws and full traceability across each raw material's production chain.
The overarching goal of this research is to comprehensively investigate the activities of the Amazonian Oils Blend through ex vivo and in vivo studies, demonstrating its effects on sensitive skin responses, interleukin 6, beta-endorphin release, redness, soothing effect, and microbiome balance.
MATERIALS AND METHODS
We conducted ex vivo tests to validate the influence of the Amazonian Oils Blend, juxtaposing its effects with those of CBD, with a specific focus on the pivotal endpoint of beta-endorphin release.
Subsequent in vivo investigations were undertaken to affirm the efficacy of the blend in addressing sensitivity issues. These studies involved the application of a lactic acid protocol, commonly known as the stinging test. Comprehensive endpoint measurements were conducted both before and after the application of the product at two time points—initially on Day 0 and subsequently on Day 28. The parameters assessed encompassed crucial aspects such as redness, skin soothing, IL-6 secretion, and the dynamic evolution of the skin's microbiota.
Ex vivo studies protocols
For the inflammatory skin model, human skin explants (2 cm x 2 cm) from abdominal plastic surgery of a female 50-year-old donor were used. These explants were topically treated with the active blend (Amazonian Oils Blend) or CBD at 3 and 5% formulated in a standard cream gel at D0, D1 and D2. At D2, they were exposed to inflammatory condition (100 µM lipoteichoic acid).
For the non-inflammatory model, human skin explants (2 cm x 2 cm) from abdominal plastic surgery of a female 49-year-old donor were used. The explants were topically treated with the active blend (Amazonian Oils Blend) at 3% or placebo formulated in a standard cream gel at D1, D2, D3 and D4 as shown in Table 1.
In both models, medium and tissue were sampled at D5 to undergo beta endorphin quantification (ELISA assay, according to the manufacturer’s instructions). Evaluation was performed also in comparison to the control.
Clinical study protocol
A double-blind controlled clinical study engaged 21 panelists with sensitive facial skin, exhibiting a positive response to lactic acid, predisposing them to skin irritation and erythema. All subjects participating in the study gave their signed, informed consent, according to GCP guidelines. Evaluations were conducted at four timepoints: D0, D7, D14, and D28.
Skin sensitivity was appraised using a stinging test and a pre-determination scale ranging from 0 to 5. The stinging test involved applying a 10% lactic acid solution to the nasolabial fold for 5 minutes, assessing itching intensity on a subjective scale (0 to 5, 5 being very severe sensations) [11]. Through a specific questionnaire, volunteers reported sensations of burning, stinging, itching, tautness, erythema, and scaled them. Erythema was measured using a colorimeter, determining the redness intensity through the a* parameter on the CIELAB color space's green-red axis. The higher the a* value, the stronger the erythema. Additionally, high resolution macroscopic pictures were obtained using a professional photography studio setup, including a Camera Nikon D5600 with polarization gelatin of flashes and a HeadScan Bench Light Face (Orion Concept, France). IL-6 levels were indicative of the anti-inflammatory effect, measured using swabbing and an ELISA kit.
Skin microbiome was evaluated through 16S rRNA genes sequencing technique focusing on the main bacteria genus indicative of sensitivity, involving sterile swab collection from participants, DNA extraction, amplification, and bioinformatics analysis. Diversity and the impact on specific strains abundant in sensitive skin were assessed using the Shannon index, metagenomics, and bioinformatics. Statistical analysis, with a significance level of p<0.05, was done using Microsoft Excel and GraphPad Prism Software, employing t-student tests for intergroup comparisons. The study included 11 randomly chosen volunteers, ensuring robust statistical validity.
Formulation applied
For the clinical study, a proper cosmetic formulation (Placebo and Amazonian Blend of Oils) was applied (Table 1). Application was done twice per day on hemi-faces, thanks to a double-blind randomized protocol.
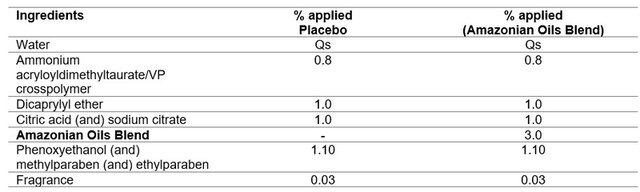
Table 1. Cosmetic formulation for Placebo and Amazonian Oils Blend applied in clinical study.
RESULTS AND DISCUSSION
Exploring the cannabimimetic efficacy of the Amazonian Oil Blend on the release of beta-endorphins in both inflammatory and normal skin conditions
Under inflammatory conditions induced by Lipoteichoic Acid (LTA), the active blend exhibited superior efficacy at both 3% and 5% concentrations. The release of beta-endorphin was significantly higher compared to CBD, showcasing a robust increase of +52% and +74%, respectively, in contrast to CBD's more modest +24% and +36%, as depicted in Figure 1.

Figure 1. Evaluation of β-endorphin release in inflammatory condition (LTA – lipoteichoic acid): comparison of the effects of the active (Amazonian Blend of Oils) applied at 3% and 5% vs. cannabidiol (CBD) applied at 3% and 5%.
In a non-inflammatory setting, the active blend at 3% demonstrated an increase in beta-endorphin release by skin explants, by +19%, as illustrated in Figure 2.
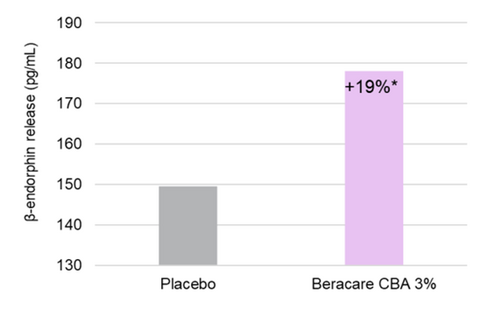
Figure 2. Evaluation of β-endorphin release in non-inflammatory condition: comparison of the effects of the active (Amazonian Blend of Oils) applied at 3% vs. placebo.
The underlying mechanism of action for the Amazonian Blend of Oils can be attributed to the beta-caryophyllene agonist interaction with the cannabinoid CB2 receptor, a well-described phenomenon [12]. Additionally, the blend, rich in linoleic acid, ensures the optimal maintenance of beta-caryophyllene on the skin surface, targeting CB2 receptors in both the epidermis and dermis. This interaction prompts the release of the neurotransmitter beta-endorphin, contributing to enhanced skin comfort.
Studies by Su et al. demonstrated in a rat model that CB2 agonists significantly elevate beta-endorphin protein levels in inflamed tissues through peripheral µ-opioid receptors and subsequent CB2 receptor activation [14].
Similarly, Ibrahim et al. observed, through a thermal stimulus model, that CB2 receptor activation stimulates the release of beta-endorphin from keratinocytes, activating local neuronal mu-opioid receptors to inhibit nociception [15]. Notably, CB2 receptor activation can induce peripheral antinociception without Central Nervous System side effects, leading to improved skin conditions.
β-endorphins, integral to the opioid receptor agonist system with the highest affinity for the mu receptor, exert a potent analgesic effect surpassing that of morphine. Operating primarily on G-protein coupled mu opioid receptors, they present a promising avenue for enhancing skin well-being [16].
Through CB2 modulation, the Amazonian Oils Blend decreases IL-6 release to lower irritation reaction
Following 28 days of daily application of the cream-gel formulation containing the Amazonian Blend of Oils, an evaluation of interleukin-6 (IL-6) quantification was conducted. IL-6 levels are intricately linked to inflammatory signs both in accute and chronic reactions. We observed a decrease in IL-6 content at the surface of the skin, particularly noteworthy when compared to the Placebo group, as depicted graphically in Figure 3. This signifies effective management of IL-6 secretion by the Amazon Oils Blend.
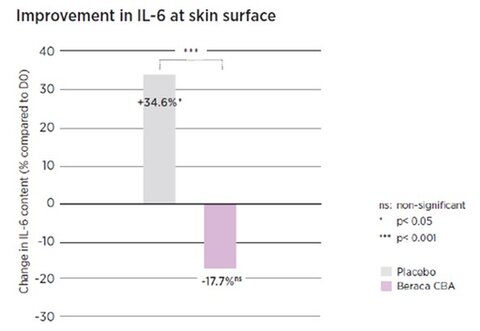
Figure 3. Quantification of IL-6 compared to D0 of the Placebo and Amazonian Oils Blend after 28 days of product use.
CB2, intricately linked to the immunobiology of skin cells [13], undergoes modulation after interaction with the Amazonian Oils Blend. This modulation facilitates a controlled release of inflammatory cytokines, leading to a consequent decrease in IL-6 levels, responsible for redness on skin surface.
Moreover, the inhibitory effects of β-endorphins on immune responses play a crucial role. Quantities of certain cytokines, including the anti-inflammatory IL-4, increase in response to β-endorphin, providing an additional layer of immune modulation [17]. This comprehensive analysis underscores the multifaceted impact of the Amazonian Oil Blend on irritation mediators.
Amazon Oils Blend leads to a visual and sensory improvement in sensitive skin
In the clinical evaluation, the Amazonian Oil Blend exhibited consistent improvement in skin sensitivity under lactic acid stress at all time points, surpassing baseline (D0) and demonstrating significant efficacy compared to the Placebo, particularly after 14 and 28 days (Figure 4). Notably, there was a remarkable 71% reduction in clinical sensitivity after 28 days. This improvement surpassed the placebo formulation by more than 50%.
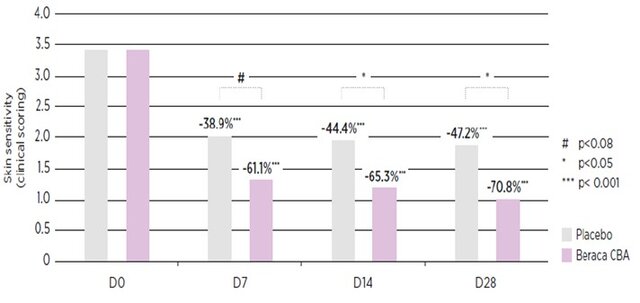
Figure 4. Comparison of the Clinical Score for skin sensitivity at D0, D7, D14 and D28 after daily application of the cream with Amazonian Oils Blend vs. placebo, after stinging test.
The reduction in redness intensity was quantified after 28 days, revealing a significant decrease of 8.5% in the a* parameter, as depicted in Figure 5.
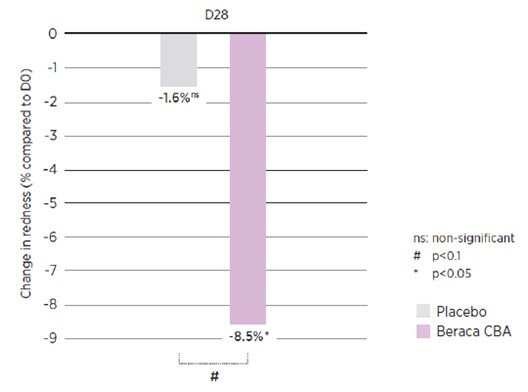
Figure 5. Redness reduction in % compared to Placebo after 28 days of use of the Amazon Blend of Oils applied at 3%.
Consequently, there was a discernible decrease in erythema, as it can be shown on one representative volunteer in the images presented in Figure 6.
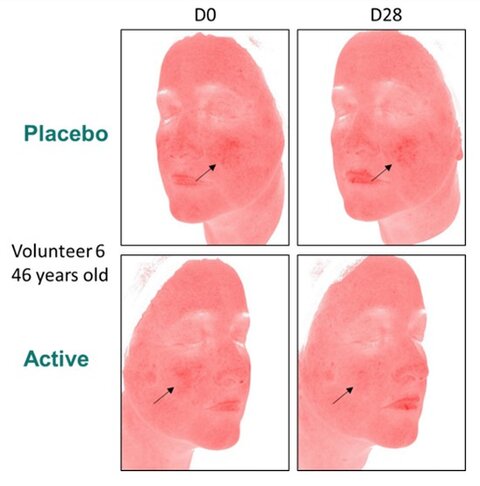
Figure 6. Picture of the volunteer 6 (46 yo), and comparison of erythema through photograph of the Placebo effect (no decrease of erythema) and the use of the Active (Amazonian Oils Blend) after 28 days of use.
The unique composition of the Amazonian Oils Blend, enriched with beta-caryophyllene, exhibited potent anti-inflammatory activity, resulting in a substantial decrease in redness, itching, and discomfort associated with sensitive skin. The 28-day application of the cream-gel at 3% concentration contributed to visible calming and soothing effects, attesting to its impact on the inflammation cascade inherent in sensitive skin's natural reactivity. This study confirms the positive effects of the Amazonian Oil Blend, providing both visual and sensory relief in individuals with sensitive skin.
The Amazon Oils Blend rebalances sensitive skin microbiota to help recover microbiome harmony
In our comprehensive evaluation, tracking the progression of sensitive skin microbiota from the initial period (D0) to 28 days (D28), distinct findings emerged when comparing the effects of the Placebo and Amazonian Oil Blend. The % relative abundance data for each genus, along with the main differences, are illustrated in Figure 7.
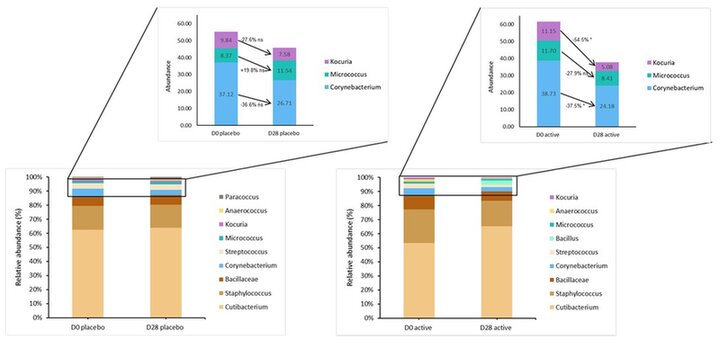
Figure 7. Relative abundance (%) comparison between D0 and D28 for Placebo and for Active (Amazonian Oils Blend) of main genera related to sensitive skin, based on our internal studies of proteomics.
Between D0 and D28, while there was a non-significant modulation in the Placebo group, the Amazonian Oil Blend application yielded significant decreases in the abundances of Kocuria (-54.5%), and Corynebacterium (-37.5%). Though the decrease in the abundance of Micrococcus (-27.9%) is not significant, the placebo lead to an increase in this population. Notably, the blend effectively mitigated the proportions of these three genera, commonly found in sensitive skins (Figure 7).
Crucially, the maintenance of a consistent population profile of the microbiota after product use highlights the blend's ability to preserve a balanced skin microbiome.
This holistic approach underscores the impact of the product on the sensitive skin microbiome. While consensus is lacking on specific bacteria genera directly influencing skin sensitivity microbiota, some prevalent at dry sites, such as Propionibacterium, Corynebacteria, Staphylococcus, Streptococcus, and Acinetobacter, are noted [18, 19].
Focusing on three specific bacteria groups (Kocuria, Micrococcus, and Corynebacterium) and assessing their impact after 28 days of daily product use, discreet decreases were observed, with a more significant reduction in the Kocuria genus—a gram-positive bacteria normal to human skin but potentially pathogenic in immunocompromised individuals [11]. Importantly, this study provides substantial evidence for the significant decrease in certain genera present in sensitive skin (e.g., Kocuria), highlighting the blend's role in preserving a healthy microbiome in sensitive skin.
CONCLUSION
While the phytocannabinoid CBD exhibits noteworthy benefits in alleviating discomfort associated with sensitive skin, its inclusion in products introduces additional psychoactive compounds, thereby contributing to the ongoing controversy surrounding its use. The soothing effects of CBD are attributed to its agonist activity on the cannabinoid receptor CB2. In response to this, we have innovatively formulated a blend comprising ethically and sustainably sourced Brazilian oils, particularly rich in beta-caryophyllene. Serving as a natural agonist for CB2, beta-caryophyllene proves to be more efficacious than CBD, inducing the release of beta-endorphin under both basal and inflammatory conditions, a phenomenon substantiated by robust clinical evidence supporting the demonstrated preclinical efficiency. Moreover, our active blend demonstrates a multifaceted approach by not only rebalancing the skin microbiota and reducing erythema through modulation of the Corynebacterium genus, elevated in sensitive skins, but also enhancing skin comfort through the mitigation of inflammatory cytokine production. In presenting this alternative to CBD for cosmetic and dermatological applications, our active ingredient stands as a viable solution, offering benefits in alleviating skin pain and discomfort while concurrently restoring equilibrium to the compromised skin microbiota.
Surfactant Applications
The application area lends itself particularly well to the use of AI. Active today in this area is the US company Potion AI (6). The company provides AI-powered formulation tools for beauty and personal care R&D. Their offerings include Potion GPT, next generation ingredient and formula databases and AI document processing. Potion’s work could have a significant impact on the entire surfactant value chain, from raw material suppliers to end consumers. By using their GPT technology, they can help target work toward novel surfactant molecules that have optimal properties for specific applications. By using their ingredient and formula databases, they can access and analyze a vast amount of data on surfactant performance, safety, and sustainability. By using their AI document processing, they can extract and organize relevant information from patents, scientific papers, and regulatory documents. These capabilities could enable Potion AI's customers to design and optimize surfactant formulations that are more effective, eco-friendly, and cost-efficient. A particularly interesting application for this type of capability is deformulation.
Deformulation is the process of reverse engineering a product's formulation by identifying and quantifying its ingredients. Deformulation can be used for various purposes, such as quality control, competitive analysis, patent infringement, or product improvement. However, deformulation can be challenging, time-consuming, and costly, as it requires sophisticated analytical techniques, expert knowledge, and access to large databases of ingredients and formulas.
AI can potentially enhance and simplify the deformulation process by using data-driven methods to infer the composition and structure of a product from its properties and performance. For example, AI can use machine learning to learn the relationships between ingredients and their effects on the product's characteristics, such as color, texture, fragrance, stability, or efficacy. AI can also use natural language processing to extract and analyze information from various sources, such as labels, patents, literature, or online reviews, to identify the possible ingredients and their concentrations in a product.
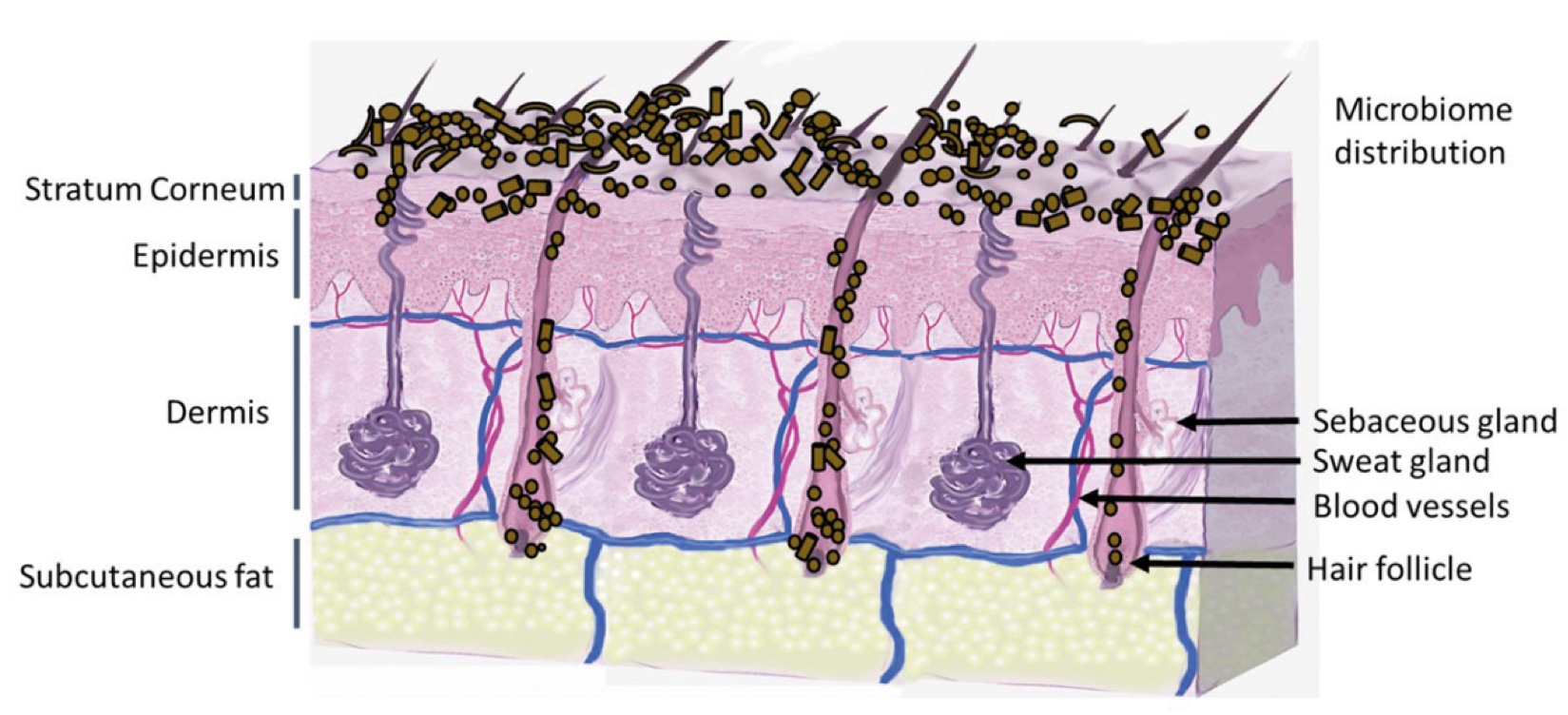
Figure 2. Skin Section with Microbiome. Most microorganisms live in the superficial layers of the stratum corneum and in the upper parts of the hair follicles. Some reside in the deeper areas of the hair follicles and are beyond the reach of ordinary disinfection procedures. There bacteria are a reservoir for recolonization after the surface bacteria are removed.
References and notes
- Inamadar, AC and Palit A. Sensitive skin: An overview. Indian J. Dermatol. Venereol. Leprol. 79:9-16, 2013.
- Tanaka, T.; Narazaki, M. and Kishimoto, T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect. Biol. 4;6:a016295, 2014.
- Qing, H. et al. Origin and Function of Stress-Induced IL-6 in Murine Models. Cell, 182,372-387, July 2023, 2020.
- Seite, Sophie. Hypothesis Letter. Skin sensitivity and skin microbiota: is there a link? Experimental Dermatology. 27:1061-1064, 2018.
- Hillion, M. et al. Comparative study of normal and sensitive skin aerobic bacterial populations. Microbiology Open. 2(6): 953-961, 2013.
- Zheng, Y. et al. Skin microbiome in sensitive skin: The decrease of Staphylococcus epidermidis seems to be related to female lactic acid sting test sensitive skin. Journal of Dermatological Science, v.97, n.3, p.225-228, 2019.
- Keum, H.L. et al. Structures of the skin microbiome and mycobiome depending on skin sensitivity. Microorganisms, 8, 1032, doi 10.3390, 2020.
- Frosch, P.; Kligman, A. and Duhring. A method for appraising the stinging capacity of topically applied substances. J. Soc. Cosmet. Chem. 28(5):197-209, 1977
- Fillaire, F. et al Alternative in vitro models used in the main safety testes of cosmetics products and new challenges. Intl. Journal of Cosmetic. Sci,l
- Jarrin et al. Sensitive Skin: Insight Into Microbiota Composition and Comparison with Microbiota of Normal Skin. IFSCC Magazine. 23(1):45-54, 2020
- Kandi, V. et al. Emerging Bacterial infection: identification and clinical significance of Kocuria species. Cureus 8(8): e731, 2016.
- Sharma, C. et al. Polypharmacological properties and therapeutic potential of β-caryophyllene: a dietary phytocannabinoid of pharmaceutical promise. Curr. Pharm. Des.; 22 (21):3237-64. 2016
- Tóth, K. F. et al. Review: Cannabinoid signaling in the skin: therapeutic potential of the “C(ut)annabinoid” system. Molecules. 24; 918. 2019
- Su, T. et al. Cannabinoid CB2 receptors contribute to upregulation of β-endorphin in inflamed skin tissues by electroapuncture. Molecular Pain. 7:98, 2011.
- Ibrahim, M.M. et al. CB2 cannabinoid receptor activation produces antinociception by stimulating peripheral release of endogenous opioids. PNAS, vol. 102, 8, 3093-3098, 2005.
- [Pilozzi, A.; Carro, C. and Huang, X. Roles of β-endorphin in stress, behavior, neuroinflammation, and brain energy metabolism. Intl. J. Mol. Sci., 22,338, 2021.
- Gein, S.V. and Gorshkova, K. G. Evaluation of the effect of β-endorphin on IL-4 and ƴ-IFN Production by CD4+ lymphocytes. Bulletin of Experimental Biology and Medicine, 146.447-450, 2008.
- Loomis et al. A mixed community of skin microbiome representatives influences cutaneous process more than individual members. Microbiome, 9;22. 2021.
- Cogen, A.L.; Nizet, V. and Gallo, R.L. Skin microbiota: a source of disease or defence? Br.J.Dermatol., 158(3): 442-455, 2008.

